As the novel coronavirus traversed central China and made its way across the seas to wreak havoc in Europe and the Americas, there were those in Kenya who wished the calamity would also befall us. My cousin Lyn, who works for a medical charity, was appalled to hear an official of the Ministry of Health express the hope that SARS-CoV-2 would arrive on Kenyan shores “tupewe pesa” — so that we can be given money. That was in February 2020; less than a month later, that maleficent official’s prayers had been answered and the funds soon followed in COVID-19’s wake, to be swiftly embezzled by Ministry of Health officials in cahoots with the directors of hastily incorporated tenderpreneurial companies. It can be safely assumed that the avaricious official was well positioned to be a prime beneficiary of the windfall.
It seems a long time ago now, when a wave of indignation swept through the nation as the news broke that funds and equipment meant to help Kenyans weather the COVID-19 storm had been stolen. Here in the Nyandarua County countryside, hawkers of hastily tailored cloth masks selling at a hundred shillings apiece soon exchanged them for the now ubiquitous sky-blue face masks once they became more readily available on the market, selling the prophylactics at ten shillings each.
The initial anxiety brought on by news of the sudden death of a middle-aged woman in May from COVID-19 two dozen kilometres further down the road from us gradually abated as it became evident that her death did not augur a hecatomb. Little by little, as the year wore on, life returned to a semblance of normal; the masks slipped off, the soap and water dispensers in front of the shops stood unused, market days returned and the police retreated to their usual occupation of extorting matatus and boda bodas. Pandemic fatigue had set in.
Over in Laikipia West, in Marmanet, my friends Patrick and Dorothy had been fanatical about sanitising ever since the news broke that the pandemic had reached Kenya. You were met with soap, water and sanitiser at the gate, a good hundred yards from their house, and the exchange of news about the weather and the state of the crops took place on the veranda under the shade of the creeping jasmine and honeysuckle.
Then early this January Dorothy called to tell me that Patrick had been hospitalised with acute pneumonia and I feared the worst. Patrick wouldn’t go to hospital when he first felt unwell and by the time it became obvious that he needed urgent medical attention, he couldn’t walk. He’s a very big man, overweight, and so Dorothy put a mattress down in the back of their pick-up truck, laid Patrick on it with the help of neighbours and drove through the night to a private hospital 30 kilometres away. Updates from the hospital were not reassuring; Patrick had contracted COVID-19 and his lungs were in pretty bad shape so he was put on oxygen. Tests also found his heart deficient and his liver malfunctioning. Miraculously, ten days later, Patrick was discharged from hospital with strict instructions to drop weight.
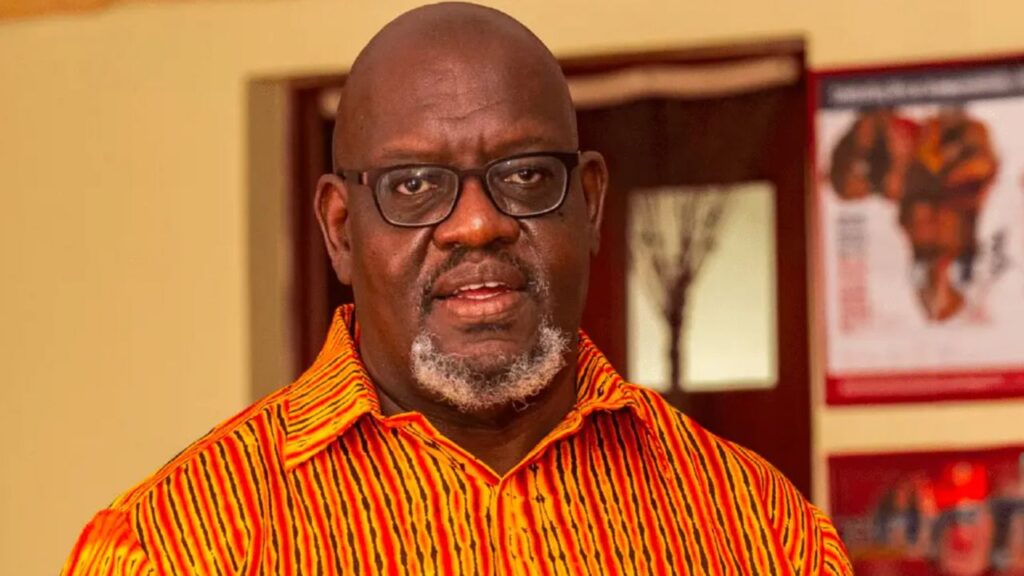
I was relieved to hear the good news and selfishly thankful that Patrick and Dorothy are an hour away from me; to my knowledge, no neighbour of mine had yet contracted the deadly disease. Then in mid-March my friend Isaac fell ill. Aches and pains all over the body, shortness of breath, dry cough, raging headache, no appetite. All COVID-19 symptoms. Isaac is an ordained pastor and missionary, bringing help and succor to the least among us, his days filled with meeting people and finding solutions. A week of treatment did not improve his condition and Isaac was hospitalised at a private clinic in Nyahururu. I feared for him and I feared for all of us who have been cozily ensconced in our personal cocoons that have given us a false sense of security that we shall be spared the COVID-19 scourge.
The small private hospital where Isaac was admitted is not testing for COVID-19. Patients also have to go to a private facility in Nyahururu town for chest x-rays. But the level of care is beyond reproach and the medical staff attentive. The young woman doctor treating Isaac seemed experienced beyond her years, explaining Isaac’s prognostic profile with clarity and taking critical decisions with authority, all the while imparting a sense of hope that Isaac would make a full recovery.
Hearing that Isaac had been taken ill and hospitalised, a young woman who had been a beneficiary of Isaac’s sustained efforts to uplift the lives of the poor of Ngobit and give their children a fighting chance by supporting their education, came running to his bedside. Nancy* had successfully completed her nursing course and was now stationed at the Nyahururu County Referral Hospital, a stone’s throw away from where Isaac was laying on a hospital bed fighting for every breath. She arranged for Isaac to be tested for COVID-19 at the government facility and insisted on paying for the cost herself.
That Nancy offered to pay for the cost of the test is testament to the regard with which she holds Isaac. Nancy has not been paid since early December 2020 when she received five months’ salary arrears. She is one of a cohort of nurses that was hired by the Ministry of Health in June 2020 in the face of the pressures brought on the medical sector by the COVID-19 pandemic. A Zoom interview was quickly followed by a job offer and Nancy arrived at the Nyahururu County Referral Hospital in early July to find that the Kenya Medical Training School lecture rooms had been converted into COVID-19 wards. But they were soon closed down and COVID-19 cases returned to the general wards once the KMTC students resumed classes in January.
Nancy tells me that there is no isolation ward at Nyahururu County Referral Hospital; surgical and medical cases are housed under one roof in the male ward and the same goes for the female ward, where female patients with gynaecological issues are also admitted. Patients with COVID-19 are “put in beds in a corner of the ward”, as Nancy heartbreakingly put it. There they wait until a doctor with Personal Protective Equipment can attend to them, administering the care that the nurses daren’t, for fear of contracting the virus. There is not enough PPE for the nursing staff; the county surveillance officer doles them out as parsimoniously as he does the COVID-19 test which is reserved for patients displaying symptoms and those with whom they have been in close contact. Nancy says that their only protection is “prayers, masks and sanitising”. Nancy says that “we are not doing things the right way but it is the management that is failing us.”
There is no critical care unit at Nyahururu County Referral Hospital. In fact, there is no critical care unit in the whole of Laikipia County. Not in the public hospitals. Not if CCU is understood to mean the availability of life support equipment and medication, and highly trained physicians, nurses and respiratory therapists specialised in caring for critically ill patients.
At the Nanyuki Teaching and Referral Hospital — the only other major public hospital in Laikipia County — there is a building whose façade bears the name Critical Care Unit but that is all the building is, a façade. Speaking at the facility on the 23rd of June 2020, Laikipia Governor Ndiritu Mureithi announced to the press that “we are preparing a 6-bed ICU and a 12-bed HDU”, adding that “the most important issue is ventilators, five of which were already at the Nanyuki hospital while another five were foreseen for the Nyahururu facility. Well, Nancy says that between June and December 2020, the only ventilators in use in the temporary isolation wards set up at the Nyahururu County Referral Hospital had been borrowed — together with the beds — from other public medical facilities in Laikipia County. The beds and ventilators were to be returned whence they came when the isolation wards were shut down in January.
The January to March 2021 issue of the Nanyuki Teaching and Referral Hospital Quarterly publication reports that “we now have also completed at 17-bed critical care unit with 6 beds reserved for intensive care unit (ICU) and now have just obtained an anaesthesiologist to get the service set up and running. A nurse has been sponsored by the hospital to specialise in critical care, and more will continue to be developed in this manner.” It is unclear which “ultramodern intensive care unit” was “unveiled” by Governor Muriithi in June 2020.
Nancy tells me that, because the Nanyuki hospital does not have the facilities, critical COVID-19 cases at the Nyahururu hospital are referred to Nakuru Level 6 Hospital in Nakuru County. If there is no room there, patients are pointed in the direction of the Kenyatta University Teaching, Referral and Research Hospital. But relatives must first deposit KSh200,000 with KUTRRH before the patient can be admitted there. The elderly mother of a colleague of Nancy’s who contracted COVID-19 last November could find no help beyond being put on oxygen at the Nanyuki hospital and so the family raised money and had her treated at a private facility in Thika. She survived.
Nancy’s cohort was not trained in the care of COVID-19 patients. They were dropped in at the deep end – the deep waters in which they outnumbered their colleagues of long standing who have permanent and pensionable contracts. Nancy and her colleagues were offered 3-year contracts with a basic salary and no benefits take it or leave it. They took it.
Last December Nancy’s cohort was split in two and she found herself in the Universal Healthcare group (UHC), falling directly under the Ministry of Health. She has not been paid since, while her colleagues who fall under the responsibility of the Laikipia County Government have been receiving their salaries every 27th day of the month like clockwork. Nancy says she doesn’t know the criteria that was used to split the group. She says that she and her UHC colleagues often call on the understanding of their colleagues who are on the county government payroll for financial help. Which is why her offering to pay for Isaac’s COVID-19 test is so significant.
Now it seems that the Ministry of Health has lost their paperwork. Their files have “disappeared” and so they cannot be paid. Nancy and her UHC group have been asked to resubmit all their diplomas, certificates and all other supporting documents. Each document must be certified by a magistrate as conforming to the original. The magistrate at Nanyuki charged 50 shillings the copy, a small enough sum until you take into account the number of documents that must be submitted and the number of nurses submitting them. And the fact that none of them have been paid since the 4th of December 2020. The county government took possession of the resubmitted documentation for onward transmission to Afya House but could not tell Nancy and her colleagues when they might expect their salary arrears to be paid.
Thankfully, Isaac tested negative for COVID-19. He had suffered a particularly nasty bout of pneumonia. He is out of the woods and back home where he haltingly (talking still makes him breathless) admitted to his wife that in the dark hours of a particularly difficult and frightening night he had yielded to his God, leaving his family in the care of the Almighty.
–
* Name has been changed.