In the wake of COVID-19 vaccine mandates (in which governments require citizens to be vaccinated regardless of their preferences), moral issues need to take centre stage. This is because we human beings are not simply matter, but also rational consciousness – we think and feel, and so it matters how we treat other people, and also how they treat us. Morality is the judging of human action in terms of rightness and wrongness, and human traits of character in terms of virtue (desirable quality) and vice (undesirable quality). While in everyday usage “morality” and “ethics” are considered to mean one and the same thing, we also use the term “ethics” to refer to philosophical reflections on morality, and this latter sense is my focus here.
Countries usually have various public health authorities that issue directives that should ideally enhance the overall well-being of their citizens. In Kenya, for example, the National Environment Management Authority (NEMA), the Kenya Bureau of Standards (KEBS), the Pharmacy and Poisons Board (PPB), and the Ministry of Health are among such bodies. Thus, the various COVID-19 protocols from the Ministry of Health are public health measures rather than medical care ones. At the global level, public health measures are currently mostly formulated and implemented under the auspices of the World Health Organisation (WHO).
As Hirschberg, Littmann and Strech explain in the edited volume Ethics in Public Health and Health Policy, central to both medical care (for ill individuals in health facilities) and public health measures (instituted by governmental authorities for the overall welfare of society) is the notion of the right to healthcare, which encompasses multiple dimensions, and ranges from concern for individual access to healthcare to the provision of a social structure conducive to healthy living. Yet the ultimate aim of public health measures is the overall well-being of the individuals who necessarily constitute the public — there can never be a public without the individuals who constitute it. Besides, both medical care policies and public health measures ought to be formulated and implemented with a deep commitment to respecting the dictates of morality, giving rise to medical ethics and public health ethics.
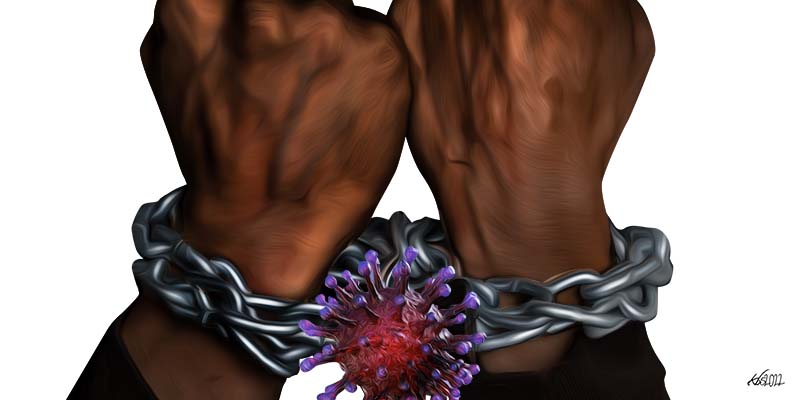
The ethical implications of COVID-19 vaccine mandates
As Hirschberg, Littmann and Strech explain, at the beginning of the nineteenth century, efforts aimed at improving and sustaining public health were primarily directed towards combating the spread of infectious diseases and plagues. However, as they further explain, the number of those falling ill and/or dying from infectious diseases was already on the decline before the discovery of the responsible pathogens (viruses, bacteria, fungi, protozoa, etc.), and the development of effective treatments and/or vaccines. Hirschberg, Littmann and Strech further observe that this marked improvement in the quality of health can be explained by improvements in socioeconomic, environmental and living conditions, greater awareness of personal hygiene, and better nutrition. They point out that the nineteenth century thus saw the emergence of the sub-discipline of social medicine that focused on the effect that conditions such as poverty and relative social status had on the public’s health. Scholars of social medicine advocated for the establishment of a healthcare system that would not only attend to those who were already sick, but also promote health for the population.
Thus, public health policies are usually designed to address prevention and health promotion. Regarding this Hirschberg, Littmann and Strech write:
[P]ublic health measures can either target behaviour and lifestyle choices of the individual, or society more generally. The former applies to Public Health programmes such as the promotion of healthy diets, abstinence from tobacco or alcohol, and participation in medical screening programmes. Examples of the latter include immunisation programmes that achieve herd immunity and projects to eradicate certain pathogens regionally, nationally, or globally, e.g. by defining targets for lowering incidence of measles or polio.
Among the many ethical issues that arise from public health measures with regard to COVID-19 vaccine mandates, I highlight five below.
Individual liberty and well-being versus the public good
There are measures that might promote the well-being of a few individuals but hurt the public, and vice versa. While, in the name of public health, many would quickly resort to the principle that the majority ought to have their way, that principle disregards the dignity (infinite intrinsic worth), agency (capacity to act) and human rights (entitlements) of the minority by treating them as though they were of relatively little significance by virtue of their numbers.
In his On Liberty, John Stuart Mill, one of the greatest champions of liberal democracy, observed that the individual ought to be protected against the tyranny of the majority in the same way as he or she ought to be protected against political despotism. In fact, while many now think democracy is rule by the majority, in Considerations on Representative Government, Mill distinguished between true democracy in which all are represented, and false democracy in which only the majority is represented. Thus, COVID-19 vaccination ought not to be a requirement on the basis of the preferences or benefit of the majority, but ought rather to be made available to all those members of the public who choose to have it without the fear of losing their jobs or their access to public spaces and services.
Freedom to accept or decline a medical procedure
The notions of human dignity (infinite intrinsic worth), human agency (capacity to act) and human rights (entitlements) have usually been acknowledged in medical care through the principle of informed consent — that the doctor is morally obligated to explain in detail the implications of any medical procedure, and to let the patient decide whether or not to receive it. Anything less than this is paternalism, that is, the treating of adults as though they were children. Since public health measures, by promoting the health of a population ought to ultimately promote the overall well-being of the individuals that constitute that population, the principle of informed consent ought not to be violated in the name of public health.
In Epistemic Injustice: Power and the Ethics of Knowing, Miranda Fricker argues that there is a type of injustice in which someone is wronged specifically in his or her capacity as a knower (“epistemic injustice”). She distinguishes two forms of epistemic injustice — testimonial injustice (the injustice that a speaker suffers in receiving deflated credibility from the hearer owing to identity prejudice on the hearer’s part), and hermeneutical injustice (suffered by people who participate unequally in the practices through which social meanings are generated). In the era of COVID-19, humanity is suffering both types of epistemic injustice, as the principle of informed consent is blatantly violated through manipulative social and traditional media, and through intimidation by public authorities issuing vaccine mandates. Indeed, populations are now regularly treated as though they are devoid of knowledge, and must therefore rely solely on instructions from political authorities purportedly to control the spread of the virus and to take care of those who fall ill from it. This approach challenges our belief in human dignity, human agency and human rights, as it reduces us to helpless, ignorant beings who must wait for government to tell us what to do, not only about our conduct in public, but also what to expose our bodies to (read “vaccine mandates”).
The individual ought to be protected against the tyranny of the majority in the same way as he or she ought to be protected against political despotism.
Currently, the narrative in social and traditional media is that the vaccine is a must, and any information about its adverse effects is quickly suppressed or explained away. This manipulative approach is evident in the talk about “vaccine hesitancy”, as though all who have so far refrained from taking the “vaccine” will eventually “come round”. A more honest discourse would have acknowledged vaccine enthusiasm, vaccine hesitancy, and vaccine rejection. Besides, the individual’s freedom is often infringed on the grounds that members of the public are not adequately equipped to make informed decisions about their own health. This amounts to treating adults as though they were children (“paternalism”). The Ottawa Charter, which focuses on patient empowerment and the strengthening of health literacy, is relevant in this regard, as is health communication, encompassing multiple levels, from the formulation of written information on specific diseases to educational campaigns aimed at the general public.
Inadequate public health communication was evident when a Kenyan citizen filed a Constitutional Petition against the vaccine mandate issued by the Kenyan government on 21st November 2021. Mutahi Kagwe, Cabinet Secretary for Health, announced that there was no vaccine mandate, and that therefore no one needed to have gone to court. At the same time, he reiterated that the unvaccinated would be denied in-person access to government services from 21st December 2021. The import of that announcement was that “There is a vaccine mandate and there is no vaccine mandate”. Furthermore, on 22nd December 2021, Health Chief Administrative Secretary Mercy Mwangangi announced that one would have to show proof of vaccination to enter public spaces such as buses, grocery stores, restaurants and game reserves. This set of statements must surely be categorised as bad public health communication.
Besides, Cabinet Secretary Mutahi Kagwe had sought to justify the vaccine mandate on the basis of the Public Health Act. However, Section 36 (d) of the Act addresses situations in which Kenya appears to be existentially threatened by any formidable epidemic, endemic or infectious disease. Yet the public health data shows that COVID-19 is not leading to massive deaths that would warrant invoking these provisions. The Public Health Act is also subordinate to the Constitution of Kenya in which the Bill of Rights is enshrined. As such, it cannot legitimately serve as a basis for COVID-19 vaccine mandates, but only for vaccine programmes. Furthermore, the dominant COVID-19 narrative emphasizes that the vaccines do not rule out one getting infected, but rather reduce the chances of hospitalization and death. Thus, vaccine-free shoppers or travellers in public transport risk their own lives, not those of fellow shoppers or fellow travellers. As such, forcing them to be vaccinated is a violation of their personal freedoms entrenched in the Constitution of Kenya 2010.
In sum, public health authorities are violating the ethical principle of informed consent by compelling members of the public to take COVID-19 vaccines. Furthermore, by making online databases accessible to a large number of people to verify the vaccination status of individuals, health authorities are also violating the principle of patient confidentiality.
Responsibility for adverse effects of vaccines
It is common knowledge that each and every vaccine has adverse effects. As such, the individual has a right to accept or decline a vaccine because it is he or she who bears any adverse effects that it may produce. Yet by enforcing COVID-19 vaccine mandates, health authorities are blatantly disregarding this important consideration. As David Ngira and John Harrington explain, a system of quality control before the deployment and use of medicines in Kenya is set out in the Pharmacy and Poisons Act, the Standards Act, the Food, Drugs and Chemical Substances Act, and the Consumer Protection Act. They however point out that none of these Acts provides for comprehensive compensation after deployment and use of vaccines. Yet any monetary disbursements that citizens might receive for adverse effects of vaccines cannot possibly restore them to their previous state of health, and must therefore be viewed more as tokens than as adequate compensation.
A more honest discourse would have acknowledged vaccine enthusiasm, vaccine hesitancy, and vaccine rejection.
What is more, observe Ngira and Harrington, to minimise liability and incentivise research and development, pharmaceutical companies require states to undertake to meet any costs arising from successful suits against the pharmaceuticals for any harm caused by vaccines. Put simply, the victims would be awarded for damages through their own taxes rather than through the profits of the vaccine manufacturers. Besides, as Ngira and Harrington also explain, in Kenya’s legal environment, victims of adverse effects from vaccines would have to demonstrate that the vaccine maker or distributor fell below widely accepted best practice, and yet acquiring the evidence to prove this and finding experts in the sector willing to testify against the manufacturer can be very difficult.
Ngira and Harrington further note that while the World Health Organisation (WHO) and the COVID-19 Vaccines Global Access (COVAX) have undertaken to honour a one-year compensation (“indemnity”) for adverse effects of AstraZeneca vaccines distributed in Kenya which allows victims to be compensated without litigation up to a maximum of US$40,000 (approx. KSh4 million), COVAX has indicated that the scheme will end once the allocated resources have been exhausted. This is a matter of concern, because there is no evidence that side effects of the vaccine fully manifest within a year. Besides, one wonders how the allocated resources for compensation were arrived at, bearing in mind that no one would have had information on how much resources would actually be needed for this purpose. Furthermore, according to Ngira and Harrington, beneficiaries of the COVAX compensation scheme are barred from pursuing compensation claims in court. COVAX also requires that before governments receive its vaccines, they undertake to pay any damages awarded to victims of adverse vaccine effects against manufacturers in any lawsuits.
The foregoing considerations lead to the conclusion that the individual, as the one who bears the full brunt of any adverse effects from COVID-19 vaccines, ought to be free to accept or decline them.
Debatable use of some primary prevention programmes
According to Hirschberg, Littmann and Strech, there is the question of the use of some primary preventive programmes such as vaccination campaigns, cancer screening, and assessment of psychological malfunctions. They further observe that problems that arise in this context include, but are not limited to, unnecessary treatment, financial interests of actors, and the role of pharmaceutical companies. For example, in Deadly Medicines and Organized Crime: How Big Pharma Has Corrupted Healthcare, Peter Gotzsche shows that drugs are the third leading cause of death after heart disease and cancer, and illustrates how pharmaceutical companies have developed toxic drugs that have caused untold suffering to many, and how law courts have awarded damages to the injured. Similarly, Neil Z. Miller discusses 400 scientific papers that show how vaccines have caused injuries, and how policy-makers ignore this information.
At the beginning of the COVID-19 crisis, the public was told that once the vaccines are developed and procured, those who receive them would be safe from the virus; then more recently it has been announced that those who are fully vaccinated will need a “booster shot” after six months. The question arises as to whether the “booster shots” are really necessary, or simply the innovation of the big pharmaceutical companies to make more profits, which would be a case of conflict of interest. Besides, it is not clear if humanity will ever be free from the vaccines if people will be required to take boosters every time a new variant emerges. What is more, while there is wide consensus among virologists on the effectiveness of natural immunity, very little is being said about this, giving the false impression that humanity’s hope only lies in the vaccines, as though humanity has not weathered numerous viruses without vaccines for millennia.
Monitoring and evaluation of public health measures
According to Hirschberg, Littmann and Strech, public health measures ought to be analysed within a framework that takes into consideration how decisions to implement the measures were reached, and how the expected impact can be evaluated and regulated effectively. As such, write Hirschberg and her colleagues, all phases of planning, implementation and evaluation of a public health measure should take into account the available scientific evidence.
In the edited volume Ethics in Public Health and Health Policy, Marckmann and his colleagues address the question of what strategies are ethically appropriate to achieve sufficiently high rates of influenza vaccination among healthcare personnel in long-term care facilities for the protection of the elderly care home residents under their charge. They contend that mandatory influenza vaccination for healthcare personnel can only be justified if the available empirical evidence on the effectiveness of the vaccine is more conclusive, and if all other less restrictive measures have failed to achieve a sufficiently high vaccination rate.
Beneficiaries of the COVAX compensation scheme are barred from pursuing compensation claims in court.
In view of the foregoing considerations, monitoring and evaluation of COVID-19 vaccine mandates ought to address the following four questions: To what extent were decisions to implement COVID-19 vaccine mandates transparent and participatory? How effective have the COVID-19 vaccines been in limiting the spread of the virus? In the light of a holistic conception of health as entailing physical, social and mental well-being, are vaccine mandates the most effective way to deal with the spread and impact of COVID-19? What is the impact of COVID-19 vaccine mandates on the overall physical, social and mental well-being of citizens?
Which way forward?
In view of the foregoing considerations, it is high time we insisted on respect for the Bill of Rights in the Constitution of Kenya 2010 that upholds the autonomy of the person and proscribes discrimination. It is high time we upheld the national principle of public participation in the formulation of public health policies. It is high time we insisted on the right to information, which implies the right to uncensored information, including free access to all shades of opinion regarding the safety or danger of taking the COVID-19 vaccines, and personal testimonies of those who have taken them, as well as reasons advanced by those who have refrained from taking them. In the end, what we are dealing with here is not simply the right to accept or decline the COVID-19 vaccines, but rather the whole range of individual freedoms, which implies the limits of state action. In sum, it is squarely within the mandate of the state to institute vaccine programmes, in which it makes vaccines available and seeks to convince citizens to receive them. However, vaccine mandates are instances of state overreach, as they violate human dignity, human agency and human rights, thereby eroding the very foundation of democratic society. If government can determine what goes into my body, what remains of my personal liberty?