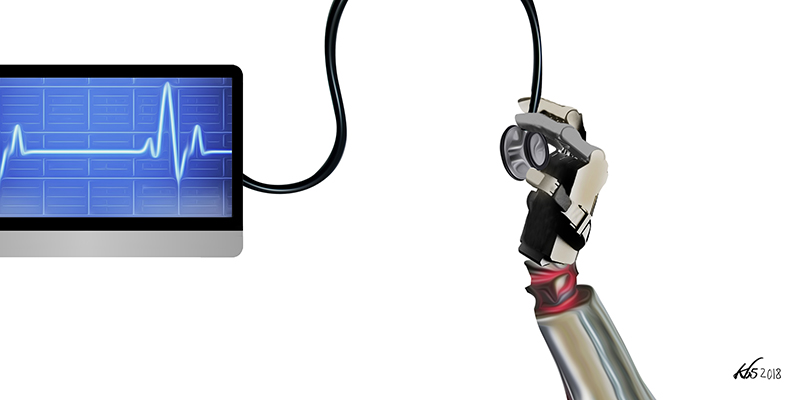
Medicine never stops evolving, and the never-ending efforts of millions of researchers around the world have provided humanity with some amazing technologies in the last few years. From artificial intelligence (AI)-based doctors that can outperform their human counterparts to the development of “smart” cancer vaccines, the race for medical innovation never stops.
However, these technologies come at a steep price, and very few countries – namely, the most industrialised ones – can afford to use them and make them accessible to the general population. Treatment disparity between the richer Western countries and the poorest African regions becomes wider every day. Countless Africans keep falling into the so-called “poverty trap”, generating a vicious circle of deterioration where ill health, epidemics, and poverty interact and mutually reinforce each other.
In an ideal world, everyone should have access to medical treatment regardless of his or her ability to pay. The reality, however, is much grimmer. When sickness occurs in a low-income household, not having the capacity to pay for medical expenses can have devastating consequences for the patient and the entire family. If access to healthcare and treatments is lacking (such as if there are no hospitals in a rural area), the individual right to health is violated, and his or her ability to work is denied. When access is granted, but the medical expenses are too steep, the consequences are no less catastrophic.
Treatment may come at the cost of financial and social well-being: the family may have to pull children out of school and push them into labour; food spending may be cut with obvious detrimental effects; and adults could be forced to work under strenuous conditions, increasing the risk of additional health issues. People who are more vulnerable to poverty are the same ones exposed to a higher risk of falling sick, such as the elderly, children, and women. Poverty increases the likelihood of becoming sick, and ill people are at a greater risk of becoming poor, generating a vicious circle that widens the disparities between the poor and the rich. When people are forced to sell what assets they have, such as livestock and land, to pay off medical debts, a financial disaster ensues, and a household may face poverty that can be dragged across the next generations. The outcome – known as the “medical poverty trap” – is a self-reinforcing mechanism that causes poverty to persist.
The medical poverty trap is particularly persistent in sub-Saharan countries such as Uganda, where low-productive agriculture, high transport costs, and small markets make the high number of rural households even more vulnerable. High economic growth rates are not sufficient to defuse the issue, however, as the cycle of health and poverty is influenced by many factors other than just economic ones. Less educated population groups are often those who have the lowest incomes, and cultural barriers can prevent them from seeking proper medical treatment when access is scarcely available. Superstition, religious beliefs, and social customs may convince them into preferring a shaman or quack over a real doctor. Ritual and herbal remedies may somewhat be part of the so-called “traditional medicine”, but they are practised with no regard to scientific procedures and are often ineffective when not directly harmful. And if the main earner of the family dies because he or she is not properly treated, the consequences for the household could be even more dramatic.
The medical poverty trap is particularly persistent in sub-Saharan countries such as Uganda, where low-productive agriculture, high transport costs, and small markets make the high number of rural households even more vulnerable. High economic growth rates are not sufficient to defuse the issue, however, as the cycle of health and poverty is influenced by many factors other than just economic ones.
Africa and healthcare – An overview of the numbers
Just a handful of few lucky individuals around the globe have access to life-saving medications and adequate healthcare. Sixteen per cent of the entire world’s population consumes a whopping 78 per cent of the total medicines produced. According to the World Health Organization (WHO), however, usage of essential medicines is similar across all countries regardless of the income category, at about between 25 and 35 per cent. This means that in low-income countries, essential medicines are used at similar rates as in higher income countries, no matter how high their price is or how burdensome it is to buy these drugs for a household. For example, to purchase the basic 7-days course of treatment with ciprofloxacin required to treat an adult respiratory infection, in Kenya a worker must pay the equivalent of over a month’s salary. In Italy, the cost of this same treatment is roughly €6, less than the hourly pay of the average unskilled labourer.
In the Millennium Development Goal (MDG) 8-E, the global community, in cooperation with pharmaceutical companies, committed to ensuring that access to essential affordable drugs would be achieved in most low- and middle-income countries by 2015. An increase in public expenditure or a widening of health insurance coverage were deemed necessary to reach this goal. Only a government may, in fact, possess the economic power to provide an entire population with sufficient coverage to afford (at least) essential drugs and treatments.
Today, in 2018, the current situation is not particularly encouraging, and most African governments are quite distant from achieving this goal. In highly industrialised countries, the average health expenditure per capita is estimated at $3100 – more than one hundred times more than in sub-Saharan Africa, where the average per capita expenditure is just a meagre $37. A single regional health centre serving 100,000 patients in a developed country administers a budget which is roughly equivalent to the budget of a country with a population of 10 million. In South Africa, to intensively treat only 60 per cent of all diabetes patients, the volume of metformin and sulfonylureas distributed by the public sector should be increased, respectively, by 366 per cent and 495 per cent. When essential drugs are not available in the public sector, patients must necessarily purchase them in the private sector at a much higher price, or forgo treatment altogether.
When only wealthier people can afford to pay for treatment, richer patients quickly become those who use the most healthcare. At the same time, newer medical technologies increase the number of treatable diseases and improve productivity by reducing illness, therefore widening socio-economic disparities. Does that mean that in low-income countries medical technologies and advancements are an enemy of equality instead of ameliorating the quality of life of the general population? The answer is no, but let’s dive in a little deeper.
The perfect recipe for disaster
Fifty per cent of children under the age of five who die of pneumonia, tuberculosis, malaria, diarrhoea, measles, and HIV across the world are in Africa. All these diseases are defined as “preventable” since they could have been easily treated if the patient had access to adequate health care services and affordable drugs or vaccines. But the average African patient must face several barriers to have access to what the international community defines as “adequate care”.
According to the World Bank, about 80 per cent of low- and middle-income Africans need to rely on public health facilities, whose situation is dire at best. Most primary care facilities suffer from a constant shortage of fundamental medications, such as in Zimbabwe, where painkillers are administered to patients suffering from all kind of diseases as a “treat-all-drug” since they are the only ones available. Patients are frequently referred to the big hospitals, but these larger facilities are limited in number, and very few families can afford to pay for their services. Many of them are inaccessible to those living in remote rural areas since they require many hours of walking in those regions where transport infrastructure is severely lacking.
Fifty per cent of children under the age of five who die of pneumonia, tuberculosis, malaria, diarrhoea, measles, and HIV across the world are in Africa. All these diseases are defined as “preventable” since they could have been easily treated if the patient had access to adequate healthcare services and affordable drugs or vaccines.
Some facilities, on the other hand, simply do not exist. Except for South Africa, in all of sub-Saharan Africa, a region where over 650 million people live, there are hardly any facilities specialising in neurology. A population that is equivalent to Europe’s and Russia’s together has little access to facilities that can be found in almost every medium-sized German, British or Spanish city.
Skilled personnel will never be available if proper training is unavailable. Even the few fortunate (and wealthy) ones who can afford the higher education required to become a specialist choose to emigrate and live in richer countries where they can hope for better wages, a superior quality of life and more chances of career growth. Still, shortage of resources and the lack of skilled personnel are just the tip of the iceberg.
For years, many African governments relied on charity projects financed by the international community to help them improve their healthcare systems. However, these plans have been mired by a constant lack of coordination, and frequently became an occasion for corrupt governments to siphon funds. The amount of resources wasted is simply depressing. For instance, over 75 per cent of all medical devices sent by Western countries remain unused because they cannot properly function outside of their natural context. The more advanced a medical technology is, the lower is the chance of it to be used properly in hospitals where no personnel have the technical expertise needed to understand its function. What’s the use of advanced digital technologies in facilities where there’s no Wi-fi or even just Internet connectivity available? The vast majority of medical devices and drugs sent cannot be transported into inaccessible areas such as deserts or inland regions, or just expire and become unusable because of the improper storage conditions. In the last decades, the “Western helping hand” did nothing but fill large warehouses with expired drugs, deteriorated vaccines and unused medical devices.
Skilled personnel will never be available if proper training is unavailable. Even the few fortunate (and wealthy) ones who can afford the higher education required to become a specialist choose to emigrate and live in richer countries where they can hope for better wages, a superior quality of life and more chances of career growth. Still, shortage of resources and the lack of skilled personnel are just the tip of the iceberg.
Most of the solutions offered by the many non-governmental organisations (NGOs) that operate in Africa seem nothing but failed attempts to patch over the shortcomings of a system that is not looking to solve its problems in the long term. For example, every time a humanitarian health crisis or a natural disaster occurs, the International Red Cross quickly implements a large mobile field hospital and dispatches many medical units to address it effectively. That’s nice, but these solutions can only momentarily solve an epidemic outburst, but cannot improve the country’s medical infrastructure or address any of its underlying issues. All those foreign specialists who voluntarily offer their services as doctors, nurses, pharmacists, and technicians may seem like angels and heroes, but their presence is too volatile to fix any of the complexities of the existing situation. As soon as the Western angels are gone, public health facilities face their usual shortages of critical drugs and devices once, and countless patients die of easily curable diseases.
Getting to the heart of the issue
Almost 20 years after the Abuja Declaration of 2001, very few African Union countries have been able to reach their target of allocating 15 per cent of their GDP to improve the health sector. Some of these countries have even reduced it. And when the funds are so low that just salary and personnel expenditures eat up to 70 per cent of hospital resources, it’s no surprise if there’s nothing left for other expenditures, such as purchasing essential drugs and medical devices, especially when the price of these medications and medical technologies is much higher in Africa than in every other well-developed country.
Understanding why this happens is the only way to cut this Gordian knot. Today, Africa produces less than 2 per cent of the drugs it consumes. Imported medications cost more than locally produced ones, and if the money invested in healthcare by the governments stays the same, this means that hospitals can buy fewer drugs, and that more sick people will die because they will not have access to the treatments they need. Africa has almost no capacity for pharmaceutical research and design (R&D) and local drug production. The only exception is South Africa, where some active pharmaceutical ingredients are produced. In every other country, even the ingredients must be imported. And the devil is in the details, because importing these ingredients would be already costly in Europe and North America, but it is ten times more in Africa, where procurement practices are plagued by a terrible transport system and general lack of adequate storage facilities.
Today, Africa imports 70 per cent of its pharmaceutical products, and many governments must spend a disproportionate amount of their already meagre resources on inefficient procurement procedures. But why can’t Africa can’t produce its own drugs like every other country (even developing ones, such as India)? Once again, there’s nearly not enough specialised personnel available. (High-scale drug production requires a high level of technical specialisation that must be supported by strong financial and educational investments – investments that repay themselves in due time, as happened in Cameroon where the $24 million-worth local generic drug manufacturer Cinpharm-Cameroon started producing antibiotics that are now much more affordable even for low-wage earners.)
Today, Africa imports 70 per cent of its pharmaceutical products, and many governments must spend a disproportionate amount of their already meagre resources on inefficient procurement procedures.
As a side note, the international community doesn’t seem to be so happy about Africa gaining its own economic independence. The biggest global pharmaceutical companies that are often so vociferous when they spend a minimal amount of their enormous fortunes to appease Africa with charity rear their ugly heads when their interests are threatened. Back in 2001, 40 pharmaceutical companies (yes, forty), among the world’s largest and most influential, dragged the South African government to court to stop it from producing generic HIV/AIDS drugs that would have significantly reduced their exorbitant prices. Eventually, most of these companies dropped the case, but thinking that they would have left millions of Africans to face certain death only to keep their profits intact is nothing less than a monstrosity.
A few words to the wise
Africa deals with 25 per cent of the world’s disease burden by spending less than 1 per cent of global health expenditure. There’s no need to assess how insufficient this amount is, especially knowing how much of it is wasted by inefficiency. Sickness means poverty; health brings growth and socio-economic well-being. It’s just as simple as that. If Africa wants to grow, it must invest in healthcare. And it must do it today, no matter how many challenges it may (and will) face.