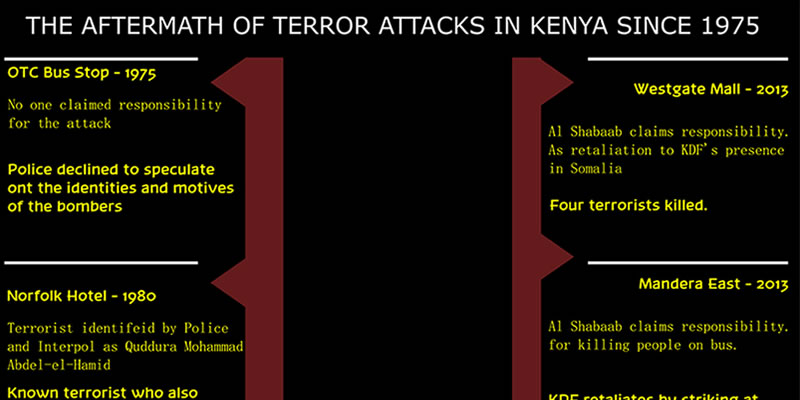
On 1 March 1975, three bombs exploded at the OTC bus stop in Nairobi. 27 people were killed and 100 others injured. No one claimed responsibility for the incident and the police declined to speculate on the identities and motives of the bombers.
On 31 December 1980, the Fairmont Norfolk Hotel was bombed by terrorists. 20 people were killed and 80 were injured after the attack. The hotel was extensively damaged and renovation commenced immediately. The terrorist, identified later by the police and Interpol as Quddura Mohammad Abd-el-Hamid, had boarded the 2.30 p.m. Kenya Airways flight bound for Jeddah via Khartoum six hours before the bomb exploded. He was a known terrorist travelling under the name Muradi Alkali with a Maltese passport.
On 7 August 1998 the U.S embassy in Kenya was bombed killing 212 people and leaving more than 4,500 wounded. The blast occurred at about 10:45 a.m.(Local time). The force of the blast blew off the embassy’s bomb-proof doors, which were later used as stretchers to carry away the injured. Injured people were rushed from the scene, as a plume of smoke rose above the Nairobi skyline. Windows were shattered as far as 10 blocks away, and bloodied clothing and papers littered the streets. On the same day, a second truck bomb exploded outside of the US Embassy in Dar es Salaam, Tanzania, causing extensive damage to the building killing 12 people.In total, the two bombings killed 224 people, including 12 Americans. The Terrorist group al Qaeda claimed responsibility for the bombings and more than 20 people have been indicted in the United States for the bombings. Eight are currently serving prison terms.
On November 22, 2002 an Israeli owned hotel In Mombasa was bombed just as two missiles were fired at an Israeli holiday jet that had taken off from the city’s airport. The missiles narrowly missed the Arkia airline plane – a Boeing 757 carrying 261 passengers – but a large part of the Paradise Hotel was reduced to rubble and the rest was a smouldering shell.15 people died. Kenya police claimed three suicide bombers were killed, along with nine Kenyans and three Israelis, two of whom were children. About 80 people, most of them Kenyans, were injured in the attack. The Army of Palestine claimed responsibility for the attacks, however, speculations arose that it could have been Al-Qaeda.
In the months of August 2007 and 2008 respectively, the Ugandan army bombed over 5,000 Turkana pastoralists in Koten in a move to flush them out of the area. UPDF was accused of bombing the Turkana pastoralists in Nakwanye (Nakwanga) and Morutorong in August 2008.
On 21 October 2010 thirty people were reported to have been killed following the night clashes between Al-Shabaab and a pro-government Somali militia on the Kenya-Somali border.
In October 2011, Kenya sent troops into Somalia after Kenya’s national security was threatened by the Somalia-based Islamist militant group, Al-Shabaab. The terrorist group had in fact carried out a number of cross-border raids during the months preceding the operation.
On October 28, 2011, Kenyan born Elgiva Bwire Oliacha alias Mohamed Seif pleaded guilty to a grenade attack in Nairobi. Elgiva Bwire Oliacha confessed to being a member of Al-Shabaab, and admitted his role in a terror attack that took place in Nairobi. One person was killed in the and 20 others were wounded after the grenade was detonated in a bar.
On 10 March 2012, Al Shabaab killed six people and wounded sixty more after four grenades were detonated at the Machakos bus station in Nairobi.
On 18 November 2012, seven passengers were killed and 33 others injured following a bomb blast in a city matatu.
On 21 September 2013, Al Shabaab attacked pedestrians at Westgate Shopping Mall. 68 people were killed and over 150 people injured over the four days siege. Witnesses claimed that the attack was highly organised, with the attackers having pre-positioned weapons throughout the building, as well as obtaining access to service elevators. Al Shabaab claimed responsibility.
On 23 November 2013, suspected Al Shabaab militants killed at least 28 people on a bus in Arabiya area, Mandera County. The heavily armed militias were reported to have waylaid a Nairobi bound bus, which left the incursion prone Mandera town early in the morning between Mandera and Arabia. According to the Mandera East sub-county commissioner Elvis Korir the assailants stopped the bus, veered off from the main road before separating passengers and targeting those they perceived to be non-Muslim. Al-Shabaab claimed responsibility for the killings through its radio station in Somalia, saying it was in retaliation for raids by the government security officials in the coastal city of Mombasa closed two mosques after allegedly found hosting radicalised Muslim youth and cache of firearms among them hand grenades.
Between 15 June and 17 June 2014, more than 60 people were killed in attacks in and near Mpeketoni, Kenya. The Somalia-based Al-Shabaab militant group claimed responsibility, but the Kenyan President Uhuru Kenyatta asserted that the attacks were organized by local politicians with ties to a network of gangs.
In July 2014, 21 people were killed in Hindi village located in Lamu county. Al Shabaab claimed responsibility.
In August 2017, anti-terrorism detectives gunned down Hussein Said Omar aka Babley, a terror suspect after a police shootout. According to police reports, Babley and his brother Ahmed Said Omar alias Dogo were both suspected to be behind the 2014 Mpeketoni massacre.
On November 21, 2014, 28 people were killed after suspected Al-Shabaab militants attacked a Nairobi-bound bus in Omar Jilo, in Mandera County. Witnesses said the attackers ordered all off the bus, divided the passengers along ethnic lines – Somali and non-Somali, shooting all non-Somalis. Many of the deceased were teachers. Al Shabaab claimed the responsibility of the killing of the 36-non local Kenyans at a quarry in Koromei area near Mandera in the night of December 1, 2014 through a pro-Al-Shabaab website. They claimed that the attack on Koromei was part of series of attacks executed by the Mujahidin to serve as a response to Kenya’s occupation of Somalia and the killing of innocent Somalis.
On April 2, 2015, Al Shabaab gunmen attacked Garissa University killing 148 people. Among the deceased,142 were students.
On July 7, 2015, Al Shabaab attacked Mandera town, throwing grenades into the homes of quarry workers. 14 people were confirmed dead. Al Shabaab claimed responsibility, declaring they were specifically targeting Christians in the attack to avenge killings of Muslims in Somalia and Kenya by Kenyan security forces.
On October 25, 2016, Al Shabaab gunmen attacked Boshari Guest house during the early morning hours. 12 people were killed. Al Shabaab claimed responsibility, claiming there target were Christians.
On November 6, 2017, Al-Shabab militants ambushed and burnt down two police land cruisers in an attack in Daba City, Mandera County. The two vehicles carrying police officers were escorting a bus to Mandera when they were hit by rocket-propelled grenades. 12 killed, several wounded.
On August 13, 2017, Al-Shabaab destroyed a Kenyan police vehicle which was driving through Yadi, Damase and El Wak towns in Mandera with an improvised explosive device. Fatalities were recorded.
On September 25, 2018, Al-Shabaab militants claimed to have overrun a Kenyan military base in Taksile area north of Pandaguo, Lamu County. They killed 10 Kenyan soldiers. Kenyan military sources reported the clashes, although they claimed that 10 Al-Shabaab fighters had been killed.
On January 15, 2019 Al Shabaab attacked Nairobi, DusitD2 hotel. 21 people were killed and several other injured. About 700 people were rescued from the compound. On February 26, 2019 Director of Public Prosecutions (DPP) Noordin Haji claimed the Diamond Trust Bank (DTB) Eastleigh branch has been accused of helping to finance terror-related crimes by facilitating the withdrawal of Sh30 million by a suspect in one week to Jilib town which is the headquarters of Al-Shabaab.