Monday, 17th December 2018 was a normal day that stubbornly refused to conform to my expectations. An impulsive decision made at 3:30 PM in a 46 Matatu heading to the Nairobi city centre dramatically altered the direction of my life.
I was on my way from Inuka Kenya offices, when a gut feeling nudged me towards the Doctor’s plaza at Nairobi Hospital. I wanted to see a psychiatrist who could recommend some sleeping pills.
When I arrived at the Nairobi Hospital, the two psychiatric consultants had both closed their offices for the Christmas holidays. Feeling unsettled, I decide to seek help at the adjacent Upper Hill Medical Centre where I quickly scanned the directory board on the first floor desperately trying to locate a psychiatrist before closing time.
Too impatient to wait for the lift, I bolted up the staircase, arrived at the reception on the third floor, and to my relief, I found other patients waiting in turn.
I walked up to the receptionist who would not accept my Jubilee Medical Insurance card: “Your insurer hasn’t installed glade which should be used to raise a claim for your card. Sorry we can’t serve you,” she said bluntly while handing it over.
I was adamant and decided to press on. “Is there any other way? Can you call the insurance company so that I can be treated and you deal with the claims later?” My persistence paid off. A few minutes later, as if fate was moving mountains, I was on the phone with my insurer who found a way to resolve the challenge.
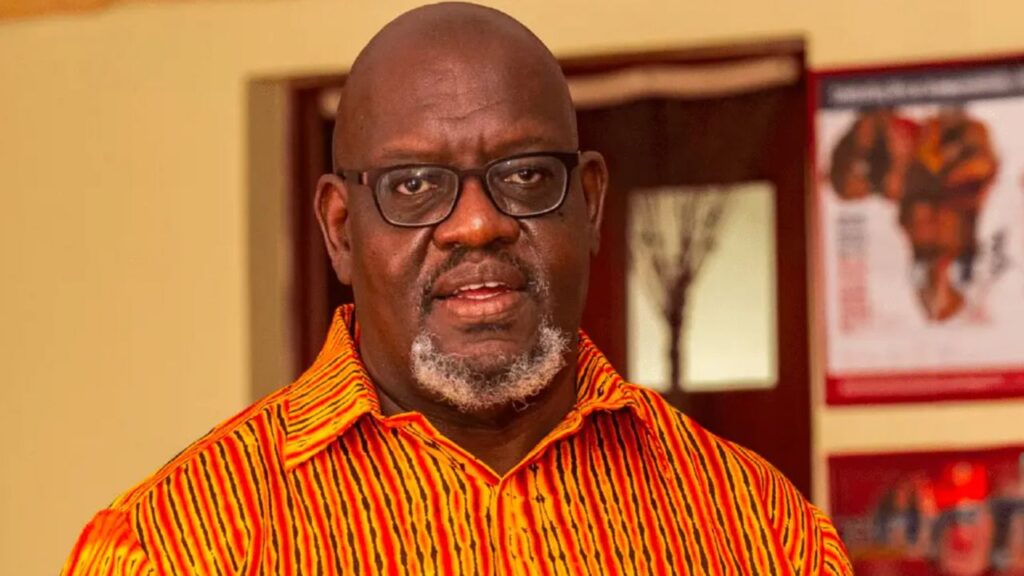
I had seen celebrated psychiatrist Dr Frank Njenga on TV. His analysis fascinated me. Only this day, I was not arriving in my capacity as a journalist to get expert opinion on a story. I was a patient.
My sleep patterns had gradually deteriorated to their worst state as far as I could recall. It had been weeks of violent nightmares. Bad people with crude weapons wanting to kill me and rogue Ikolomani Bulls chasing me through the night.
I could not outrun death and when I tried to scream for help, I found my voice frozen. I felt helpless and trapped in the nightmares. I would wake up in panic, breathless and sweaty. I wanted to see a psychiatrist who could recommend some sleeping pills just like one had done in 2014 when I had a similar experience.
Frank Njenga was wearing a clean white shirt with a blue-stripped tie. His smile and calm demeanor disarmed me on the spot. “Tell me more about yourself,” he asked after exchanging a few pleasantries.
I went on and on about my family’s history, and myself while his head was glued on my file taking notes. Sometimes he would lift his head when I said something that sounded like a trigger. “Tell me more about incident, what happened?” he would ask when I explained some of the darkest seasons I had gone through recently.
He gave me a piece of paper, which had about 30 questions and told me to tick statements that closely represented how I had lived my life. While he had hoped that I would only tick about 10 when he looked at the paper, I had ticked 25 out of 30 and that’s how he partly discovered what had been eating me. To ascertain his preliminary findings, he sent me for a cognitive test to corroborate what he was suspecting.
What I thought was just a simple sleep issue turned out to a symptom of something deeper.
“I’m glad you came here, we are going to help you,” he reassured me as we chatted for about an hour, the longest I have been in a doctor’s office.
“Odongo, we may need to take you to a place so that we can monitor your sleep and find out if there are other underlying issues,” he advised as there was sufficient evidence that I needed to be monitored.
I knew the weight of inadequate sleep and was desperate for a solution. I accepted his suggestion.
“Mental health is like an onion, we peel it from the outer layer as we dig in. That’s the only way we can find out the core of the problem,” he added.
When we arrived at the gate of Chiromo Lane Medical Centre in Lavington, I saw a disturbing sign: Visiting hours is between 9-11 am and 3-6 PM. My panic buttons went off. I was not suicidal and I did not have the urge to harm other people. I just had migraines, nightmares and an anxious mind. Why was I being admitted into a restrictive hospital?
Begrudgingly, I agreed to check in for a night. The bungalow house that sat on a lush green serene environment complimented by the friendly staff all disarmed me.
In hindsight, this was one of the best decisions, I made in my life. For the next six days, I would go through an overwhelming journey of self discovery that I was hardly prepared for.
At the end of the first day, I was diagnosed with clinical depression, mild Attention Deficiency Hyperactivity Disorder (ADHD) and trauma. Though I was predisposed to some of the disorders, a toxic work environment for five years, an emotionally abusive relationship and front row coverage of the 2017 traumatic elections as a reporter played a key role in triggering the sleeping demons that landed me in a hospital.
After I was done with a two-hour therapy session, I slowly dragged my exhausted body back to my admission room. As I sat on my bed while listening to music, a wave of emotions descended and I broke down and wept. I slowly moved from the bed and sat on the floor with my back against the wall and legs straightened. For the next three hours, I wept until I felt weak.
Kenya Mental Health Policy (2015-2030) indicates that mental disorder cases have risen exponentially in Kenya. Estimates point that 20-25 percent of outpatients seeking primary healthcare present symptoms of mental illness at any one time. There are no sufficient qualified medical personnel and facilities to take care of this lot of patients.
A 2015 performance audit report from the Office of the Auditor General (OAG) on the state of mental health paints a grim picture. As at 2015, there were only 92 psychiatrists in the country instead of the 1,533 required. 327 psychiatrist nurses instead of 7,666. The report stated that “While it’s expected that a psychiatrist should serve 30,000 citizens, currently a psychiatrist is serving about half a million citizens”.
I still count myself privileged to have gotten medical attention. The ability to afford private insurance cover, know where to go when symptoms arise and get treated by Dr. Njenga is privilege.
Millions of Kenyans who struggle to meet basic needs are exposed to mental disorder triggers stemming from their environment and cannot afford this privilege. For the poor masses in Kenya, quality primary health care is a mirage. Add the lack of specialized mental healthcare and you condemn a whole section of the population to destitution.
Mathari Hospital, which is an affordable public facility and the only hospital in the country offering specialized psychiatric services and training is in a sorry state according to the OAG. For the three financial years, 2013/14, 2014/15 and 2015/16 Mathari hospital was provided only about 30% of the funds allocated under the recurrent expenditure and nothing under the development expenditure.
As government policy, all mentally ill law offenders who require in-patient services can only be admitted in Mathari Hospital under the Maximum Security Unit regardless of severity of their condition. They make up 35 percent of the inpatients in the hospital yet there is no cost sharing to take care of them thereby straining the already limited resources.
Low funding means that apart from inadequate equipments, the wards are also insufficient with the hospital being reported to have an average bed occupancy rate of 115 percent. The low stock of critical drugs, inadequate skilled and qualified personnel to handle the patients are some of the issues plaguing Mathari as raised by the OAG report.
On the receiving end are the patients who are dependent on the hospital receive poor services including delayed diagnosis that can make the condition worse. While National referral hospitals should provide specialized healthcare services and should operate with a defined level of autonomy including a Board and a Chief Executive Officer, Mathari hospital is the only psychiatric hospital of its caliber in Kenya that operates under a department in the Ministry of Health.
The national statistics do not offer any reprieve either. County managed hospitals where the bulk of the nation relies on for mental health care is stuff of horror.
In the 47 counties, only 25 have psychiatric units. Even in the 25 counties where the services are available, they are pledged with the challenge of outdated equipment, inadequate stocks for essential drugs and insufficient personnel to treat mentally ill patients.
According to the OAG, besides Mathari national referral hospital, mental healthcare services are only available at 29 of the 284 hospitals in Level 4 and above of the referral chain. “This represents just 10% of the total facilities in Level 4 and above and 0.7% of the 3,956 government-owned health facilities,” notes the report.
A month before I walked into the hospital, I hardly thought that my relationship challenges could compound my psychological well-being. The revelations from a text message that came from my ex took me to the brink. That night, the thought of going to bed haunted me. I stayed on my couch writing until 4 am. I tried to pray but I could not. My heart was heavy.
My head was never the same after that night. It started to sound like the world’s busiest construction site. Constant hammering, grinders cutting through metal, welding machines and all sorts of construction chaos formed an unholy symphony in my head.
During the day, migraines became the norm and at night, insomnia took over. When I closed my eyes, I was battling anxiety unable to focus my attention on anything. I experienced anger, bitterness and a heavy dark cloud hovered above. I had never felt like this before.
While the public debate on mental health is welcome, as a person recovering from a mental disorder, there is need to push a wholesome discussion on the reality of the state of mental health in Kenya beyond depression.
We need to broaden the discussion to talk about different conditions and their symptoms, different medication and management of disorders. According to the World Health Organisation (WHO), there are over 10 mental health disorders affecting human beings including borderline personality disorder, anxiety and panic attacks, bipolar disorder attention-deficit/hyperactivity disorder (ADHD) among others. Depression is just one of them.
We also need to talk about inadequate mental health facilities and the few stretched mental health professionals. By solely pushing the message of depression, we downplay the reality of mental health challenges in Kenya and the manifest consequences.
Stigma and lack of accurate information continues to cost the global economy about $1 trillion every year in productivity due to depression and anxiety. WHO data, reveals that mental illness accounts for 30 percent of non-fatal disease burden worldwide and 10 percent of overall disease burden, including death and disability.
In 2016, the grim reality necessitated the World Bank Group (WBG), the World Health Organization (WHO) and other partners to kick start a call to action to governments, international partners, health professionals among others to find solutions to what is fast becoming a global mental health problem.
Leaving the hospital on 24th December, I was informed that Jubilee Insurance Company had rejected my claim for two reasons: The condition I was diagnosed with is not covered in my policy I was holding (Never mind that ADHD predisposes one to other mental illnesses like depression which they claim to cover).
For trauma and depression, which is covered under the policy, they said I needed a one-year waiting period (I took the cover in September 2018 after leaving formal employment) despite the fact that I was a previous policyholder with the same company for three years and my claim history was generally low and it didn’t have any mental illness.
I was furious because while signing the form, nobody informed me that I was entitled to a waiver. While I took time (2 weeks) to read the policy document, I didn’t notice that ADHD (I knew this condition when I was diagnosed in December) was not covered. The agent who signed me on was either too concerned with the commission or the corporate culture of the organization encourages ambiguity for profit gain.
My review of the mental health policy and the relevant laws including the Mental Health Act of 1978 and the Mental Health (Amendment) Act 2018, showed that the same clause they used to decline my claim is potentially discriminatory. The policy states in part “Ensuring that the health insurance system does not discriminate against persons with Mental, Neurological and Substance use (MNS) disorders in accessing insurance policies,”
Though not yet enacted, clause 3D(3) of the Mental health amendment bill of 2018 amplifies the 1978 Act more expressly: “A person with mental illness shall have the right of access to medical Insurance for the treatment from public or private health insurance providers. An insurance company or person providing health insurance services shall not discriminate against a person with mental illness or subject a person with mental illness to unfair treatment in obtaining the necessary insurance cover.”
As a good citizen, I appealed their decision using internal mechanism but I still hit a dead wall. I am now preparing to take the dispute before the Insurance Regulatory Authority (IRA) with a view to not only settle my bills but also to amend the discriminatory clause for personal policy holders.
Kenya grapples with a low insurance penetration rate at 2.68 percent. The 2017’s Insurance Industry Annual Report 2017 by IRA flags mistrust among the reasons listed for the cause of low rate of insurance penetration in Kenya.
As I began to investigate the nature of insurance claims for mental health cases, I have encountered numerous patients who have suffered mental health challenges and the stories are similar: A clever refusal to pay claims using technicality.
In developing countries like Kenya, the mental health landscape is often plagued with insufficient data to show the economic impact of mental illnesses. However, the effects are wide-ranging and long-lasting including the impact on the families’ and care-givers’ resources; the expenses related to crimes caused by the mental disorders; the productivity losses due to debility, morbidity and premature death; and the psychological pain borne by the patients and their family members.
There is also a correlation between the state of mental health and rise of the Sexual and Gender Based Violence (SGBV). Evidence shows that mental health has a crucial role in the primary prevention of sexual and gender-based violence (SGBV) even though most standard practice has focused on the role of mental health post-violence, and primary prevention relying on public health models that do not explicitly include mental health.
For example, research shows that empathy, self-esteem, compassion, emotional regulation and resilience, stress management, relationship building, and challenging problematic social norms are crucial for primary prevention of SGBV.
A 2016 report by the National Gender and Equality Commission estimated that the cost of GBV stood at KES 46 billion, which translated to about 1.1 percent of Kenya’s GDP due to medical related expenses, litigation costs, productivity losses among others.
More needs to be done to create awareness about mental health and its economic cost. Also, there is need for an immediate taskforce to collect data about mental health in Kenya to advise policy decisions.
In the words of Owen Arthur, former Prime Minister of Barbados: “For he who has health has hope; and he who has hope, has everything.”