The brain drain of medical professionals from African countries to rich countries in Europe, North America, and the Middle East has been particularly pronounced since the 1980s. As Bibilola Oladeji and Oye Gureje have noted, as of 2011, there were more than 17,000 African physicians practicing in the US alone, over two-thirds of whom had been trained in African medical schools. Of this group, two-thirds were trained either in Nigeria or South Africa, the two countries with the most extensive medical training systems on the continent. Psychiatrists have also made up a significant piece of the larger medical migration, drawn by higher salaries, better facilities, opportunities for professional development, and prospects for long-term stability to seek jobs outside of the continent.
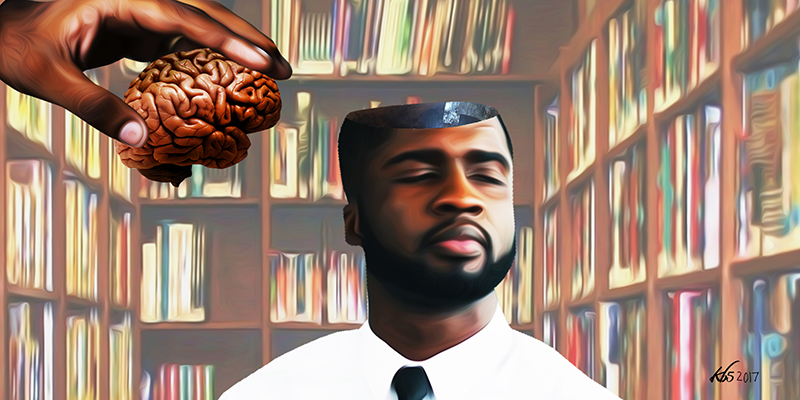
The brain drain has become a commonplace terminology to describe the emigration of highly skilled labor from developing countries to highly industrialized states in the post-colonial world. The concept has been particularly valuable for understanding persistent underdevelopment in sub-Saharan African countries as related not so much to deficiencies in African expertise as its redirection primarily for the benefit of wealthy countries. Similar to the “brawn drain” of the Atlantic slave trade or the natural resource depletion that characterized European colonialism in much of the continent, brain drain has had long-lasting impacts on African countries’ internal development and position in the global economy.
The impact of the brain drain on mental health care in Africa can be seen through the example of Nigeria, one of the few sub-Saharan African countries with university hospitals providing accredited medical training in psychiatry. Nigeria’s first trained psychiatrist of indigenous background was Thomas Adeoye Lambo, who studied at Birmingham and the Maudsley Hospital in the UK before returning to Nigeria to practice at the newly founded Aro Mental Hospital in 1954. Lambo and his acolyte, Tolani Asuni, developed much of the infrastructure of Nigerian psychiatry in the 1960s and 1970s, and several Nigerian universities began producing psychiatrists by the 1980s. The purpose of developing such programs was to produce a qualified mental health workforce for the country. Students from other countries in West Africa also trained in psychiatry at Nigerian institutions. Nigeria’s mental health care workforce grew slowly but surely from only three psychiatrists in 1955, to 25 by 1975, and 100 by 2001. But the brain drain has had a major impact on Nigerian psychiatry. Today, there are roughly 250 psychiatrists in Nigeria to serve a population of approximately 190 million. At the same time, a study from 2010 found that there were 384 Nigerian psychiatrists practicing in the US, UK, Australia, and New Zealand, a number 50% higher than the estimated total practicing in Nigeria.
The effects of this psychiatric brain drain have been significant. Beyond the worsening of the psychiatrist-to-population ratio, this phenomenon has the potential of severely weakening ongoing reproduction of this limited resource as more freshly qualified psychiatrists and senior residents are being enticed/encouraged to relocate on the guise of training opportunities abroad, from which they never return. In addition to psychiatrists, mental health nurses are also leaving the continent in droves, with packages designed to make emigration easy and more likely to be permanent. The rate of migration far outstrips the rate of production, leaving a huge deficit in human resources, one of the major pillars of a health system, according to the World Health Organization.
Several reasons have been proffered for the exodus of medical doctors from Africa to the economically developed world. Oberoi and Lin classified these reasons into endogenous and exogenous factors. Endogenous factors include poor working conditions, poor remuneration, and lack of job satisfaction and job security with little or no opportunities for career development. Exogenous factors include social pressures from relatives, preponderances of civil unrest, and armed conflicts with attendant high levels of insecurity. Ironically, the factors that push mental health care workers to relocate abroad are the same ones that likely contribute to rates of psychological distress in their communities of origin that, in turn, require more and better mental health care.
Since the late 2000s, the “global mental health” movement has sought to ameliorate this “treatment gap” in mental health services in developing countries, including Nigeria and others in sub-Saharan Africa. In most cases, reducing the treatment gap relies heavily on training lower-qualified workers to perform the duties of highly-skilled practitioners, a set of practices known as “task shifting.” Task shifting in international public health has existed for a long time, and has been employed extensively in the field of HIV/AIDS diagnosis and treatment in many environments. But it’s use in psychiatric care is somewhat more controversial. Most notably, global mental health has been critiqued as potentially socially and culturally insensitive, importing knowledge and practices from western industrialized countries that might not adequately reflect local cultural beliefs or social determinants of health, while simultaneously marginalizing indigenous health systems.
Task shifting has also been proposed as a strategy for alleviating the effects of the brain drain on the health care sector. In a review of policies to address brain drain in sub-Saharan African countries, Edward Zimbudzi has identified some areas of possible intervention. These include ethical recruitment, brain drain tax or compensation for source countries, increasing investment in training more professionals, improving remuneration of health workers and working conditions in general, importing more staff, ensuring political stability, and encouraging remittances. However, the review concluded “that there is considerable consensus on task shifting as the most appropriate and sustainable policy option for reducing the impact of health professional brain drain from Africa.” While some studies have concluded that task shifting has effectively filled the treatment gap, others have indicated that it is by no means a comparable substitute for professional mental health care due to lack of proper supervision and training of lower level workers, among other factors.
But we would like to offer a different critique of the task-shifting discourse: it’s tendency to normalize the brain drain of health care professionals. Global mental health has always emphasized practicality over ideology: anything that can be done to fill the “treatment gap” is presumably better than not doing it. The origins of the medical brain drain are not really global mental health’s concern, but its consequences are a large part of the foundation of the movement’s argument for “scaling up” the health care workforce to address the “treatment gap,” which is effectively the primary justification for the movement’s existence. However, in making the case for immediate action, the discourse on task-shifting in global mental health replicates the long history of ignoring the long-term exploitation of African resources in order to focus on short-term, externally funded, non-state interventions to provide what Africa supposedly “lacks.”
Promoting task shifting to lower cadre health care workers as the best way to scale up mental health services in low- and middle-income countries indirectly suggests that these countries cannot hope for better, even as billions of dollars are lost by African countries from investment in training highly qualified health workers who go on to treat patients in wealthy countries. Meanwhile wealthy countries acquiesce to helping train up less-qualified caregivers to fill the “treatment gap” created in part by this brain drain. It also implies that African countries can get by on less than wealthy countries. Indeed, severe mental illness continues to be neglected under the “task shifting” model that does little to increase specialist capacity to handle such cases. While this rather popular principle in global mental health appears practical, it inadvertently panders to the notion that some lives are more important than others, and calls to question the relative value placed on the health and lives of citizens of the developing countries of Africa compared to the developed world. It reinforces and normalizes global inequalities.
Mitigating the psychiatric brain drain must ultimately be about much more than filling “treatment gaps.” It must also be about addressing the geopolitical and macroeconomic conditions that have produced the gap in the first place. Developing equitable and sustainable mental health services for all Africans is a political, economic, moral, and ethical issue of contemporary urgency and historical significance.
–
This post is from a partnership between Africa Is a Country and The Elephant. We will be publishing a series of posts from their site once a week.