A recent study has revealed that expectant mothers in African countries, especially Uganda are more likely to die with preeclampsia condition compared to their counterparts in other East African countries.
Preeclampsia is a pregnancy disorder characterised by hypertension especially after 20 weeks of pregnancy. It can be dangerous to both the mother and the unborn baby. Gestational pregnancy may increase the risk of premature birth of the baby, increased birth weight of the baby, cesarean delivery, and preeclampsia.
Bulk of government health facilities in the country are struggling to manage the condition since most of the critical drugs needed to manage the condition are not stocked, simply because the government has not prioritised the condition.
The condition is the second cause of maternal deaths worldwide.
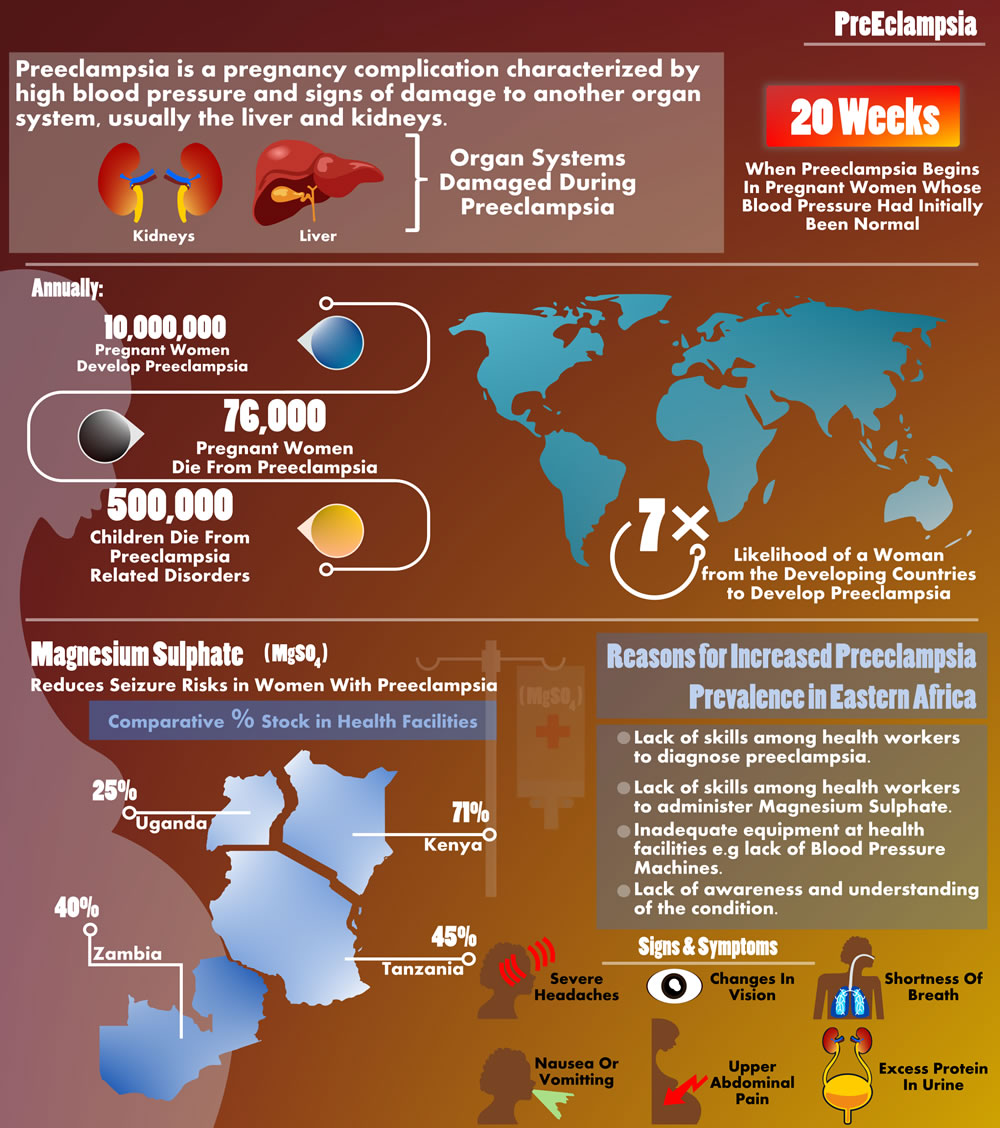
The study done by the Health Action on the situation on reproductive health commodities revealed that only 25 per cent of health facilities in Uganda stock Magnesium Sulphate as compared to 71 per cent in Kenya.
Magnesium sulphate is a mineral that reduces seizure risks in women with preeclampsia. A healthcare provider will give the medication intravenously.
The study conducted in four countries (Kenya, Uganda, Tanzania and Zambia) revealed that facilities in Tanzania and Zambia were not any better as far as the stocking of the commodity is concerned with 45 and 40 per cent respectively.
During the commemoration of world Preeclampsia Day on May 22 in Uganda, health facilities in Lira – a city in the Northern Region of Uganda – called for support from the government to enable them to handle mothers with the condition.
About 10 million pregnant women around the world develop preeclampsia each year. Out of the total 76,000 women die from preeclampsia and related hypertensive disorders. Additionally, the World Health Organisation (WHO) estimates the number of babies who die from these disorders every year to be on the order of 500,000.
In developing countries, a woman is seven times as likely to develop preeclampsia than a woman in a developed country. From 10-25 per cent of these cases will result in maternal death.
Preeclampsia should be detected and appropriately managed before the onset of convulsions (eclampsia) and other life-threatening complications.
Administering drugs such as magnesium sulfate for pre-eclampsia can lower a woman’s risk of developing eclampsia.
In developed countries like the US, pregnant women are commonly followed by a healthcare specialist (doctor, midwife or nurse) with frequent prenatal evaluations. In other areas of the world with little access to care and lower social status of women for instance in Africa, traditional health practices are usually inadequate to detect preeclampsia early.
Hypertensive disorders of pregnancy commonly advance to more complicated stages of the disease, and many births and deaths occur at home unreported.
Poor women in remote areas are the least likely to receive adequate health care. This is especially true for regions with low numbers of skilled health workers, such as sub-Saharan Africa and South Asia.
Although levels of prenatal care have increased in many parts of the world during the past decade, the WHO reports that only 46 per cent of women in low-income countries benefit from skilled care during childbirth. This means that millions of births are not assisted by a midwife, a doctor or a trained nurse.
But why are women in Africa dying of this condition yet it can be prevented?
Dr Annettee Nakimuli, an obstetrician-gynecologist at Mulago Hospital in Kampala and lecturer at Makerere University did research to answer that question.
She says although the condition affects women worldwide, in African women, it is more common and particularly severe. It also occurs earlier in pregnancy and can recur in subsequent pregnancies.
Dr Nakimuli reported that at Mulago Hospital where she works, 15 per cent of pregnancies develop life-threatening complications such as preeclampsia, hemorrhage, obstructed labour and sepsis.
She describes herself and her colleagues as being “on the front line” in the battle against death in pregnancy and childbirth. She did a study in 2017 in collaboration with Cambridge’s Department of Pathology and Centre for Trophoblast Research to unravel why a complex disease is so much worse in Africa.
But why would women of African descent suffer so much more from preeclampsia than other women? “There was an assumption in Africa that there was a socioeconomic reason, like poverty,” says Nakimuli. “I was convinced that there was something biological.”
She recruited 750 mothers at Mulago Hospital to what is the largest genetic study of pre-eclampsia conducted in Africa. She collected blood and umbilical cord samples and, in Cambridge, ‘typed’ the DNA to look at all the genetic variation.
“It was kind of a high-risk project, but my determination kept my hope alive. I wanted to find big things.” She says
The findings of the study revealed that killer-cell immunoglobulin receptors (KIRs), genes that protect African women against pre-eclampsia are different from those that protect European women.
KIRs recognises proteins called MHC on the invading fetal cells. Certain combinations of maternal KIR genes and fetal MHC genes are associated with pre-eclampsia, whereas other KIR genes appear to protect against the disease.
Moreover, the risky combination of maternal KIR and fetal MHC proteins occurs at a much higher frequency in sub-Saharan Africa than anywhere else in the world.
From the study, Dr Nakimuli together with other researchers will be researching to understand the biology of preeclampsia.
“We think that women of African ancestry may have these risk genes because of certain beneficial selective pressures, otherwise why would genes that kill mothers and babies be so common in the population? People with the gene that causes sickle-cell anaemia can fend off malaria – perhaps something similar is happening for KIR genes? And so now we are starting work to see whether the genes are protecting against infections such as measles, HIV and malaria.” She says
She also pointed out a lack of awareness and understanding of the condition as a barrier to treatment.
“There’s a general lack of awareness and understanding,” explains Nakimuli. “There isn’t even a Ugandan word for preeclampsia. The closest people get to describing the condition is ‘having hypertension which is different from other hypertension when you’re not pregnant’. It becomes a mouthful.”
Together with other researchers, they developed a format of awareness messages in which a radio presenter would play a real-life testimonial – such as a woman relaying the complications of her pregnancy – and then invite listeners to reply to a related question by sending a text to a toll-free number. Each respondent would subsequently receive an SMS socio demographic survey to complete.
“What makes preeclampsia such a challenge is that it has been impossible to predict or prevent,” explains Professor Ashley Moffett, from Cambridge’s Department of Pathology and Centre for Trophoblast Research, who is an expert on the disease.
“It’s been called the ‘silent killer’ because many women cannot feel the danger signs that their blood pressure is rising until it’s too late. Even when it is detected the only course of action is constant monitoring, and ultimately the only cure is delivery sometimes at too early a stage for the baby to survive,” adds Moffett.
However, during the release of the research study in the four countries in Zambia, Mr Denis Kibira, Executive Director, Coalition for Health Promotion and Social Development (HEPS) who conducted the study cited lack of enough blood pressure (BP) machines, designated preeclampsia ward, a postnatal ward, and inexperienced health workers to handle women with the condition as some of the challenges.
For instance, Lira Regional Referral Hospital in Uganda which receives about 100 expectant mothers daily for antenatal care, has only one blood pressure machine yet it serves nine districts in the region.
Mr Jino Okot, the in-charge of Ogur Health Centre IV, most health workers do not have the necessary skills to administer magnesium Sulphate and the government should do something to improve the situation of the mothers.
“Most of the health workers do not have the skills to diagnose preeclampsia. Some of them do not even know how to mix and administer. The Ministry of Health should understand that health workers need training if we are to ably manage the condition,” Mr Okot said.
Mr Edmond Acaka, Lira District assistant health officer-in-charge of maternal and child health, appealed to the Ministry of Health to come to the rescue of the district by increasing its budget to accommodate more of the commodities.
While Ms Beatrice Nyangoma, communications officer for HEPS-Uganda, asked the Ugandan government to consider regulating prices for magnesium sulphate to improve affordability and availability.
Mr Kibira while releasing the data to health journalists in Zambia in September said different levels of facilities were picked in each country. The methodology used consisted of a questionnaire and a qualitative survey component. Data collectors were trained in June 2018 (Tanzania), July 2018 (Kenya and Uganda), and August 2018 (Zambia).
The levels of health facilities visited in Kenya were level 3 and 5, in Tanzania: ‘Dispensary’ and above (country level 1-3), in Uganda: ‘Health Centre III’ and above (country level 3-7), and in Zambia: ‘Health post’ and above (country level 1-4).
The study conducted across sectors (public, private and mission) hospitals in urban and rural areas in 169 facilities in Kenya, 126 in Tanzania, 145 in Uganda and 237 in Zambia also revealed there was a large variability of supplements per type and country.
The mean availability of these commodities was 36 per cent in Kenyan health facilities, 29 per cent in Tanzanian, 37 per cent in Ugandan and 34 per cent in Zambian health facilities.
The data collection tool assessed the availability of 55 SRH commodities at the moment of data collection in each of the 677 study facilities.
Only in Zambia were all these supplements such as calcium gluconate, ferrous salt, folic acid, zinc, and oral rehydration salts commonly available (70-84 per cent overall) except calcium gluconate, which had an overall availability of just six per cent.
Calcium gluconate was also poorly stocked in other countries, with availabilities of 28 per cent in Kenya, 17 per cent (Uganda) and two per cent (Tanzania).
Oxytocin, used to induce labour and for the prevention and treatment of postpartum hemorrhage, was stocked relatively commonly (47-91 per cent), except the private sector in Kenya (27 per cent) and Zambia (20 per cent).
Zambia was leading with oxytocin stocks in facilities at 94 per cent followed by Kenya at 84 per cent. Tanzania third at 78 per cent while Uganda was the least with 64 per cent.
Gentamicin, used to treat pneumonia and neonatal and maternal sepsis,was moderately available in all countries (overall, 60-81 per cent), except for in Tanzania (23 per cent).
While the availability of dexamethasone, used in the management of pre-term labour to improve foetal lung maturity, was considerably lower, ranging from 11 per cent (overall, Tanzania) to 50 per cent in Uganda.
According to the World Health Organisation, the full intravenous magnesium sulphate regimens are recommended for the prevention and treatment of eclampsia.
“Magnesium sulfate is a lifesaving drug and should be available in all health-care facilities throughout the health system. The guideline development group believed that capacity for clinical surveillance of women and administration of calcium gluconate were essential components of the package of services for the delivery of magnesium sulfate,” says the WHO.
The international health agency states that in settings where there are resource constraints to manage the administration of magnesium sulfate safely in all women with pre-eclampsia, there may be a need to accord greater priority to the more severe cases.
The availability of medical devices from the study was inconsistent across the countries.
Speculums (metal or plastic device that is used to open the vagina enough to see inside were available at 85 per cent of the public facilities of Kenya, 84 per cent of Tanzania’s, 89 per cent of Uganda’s and 64 per cent of Zambia’s public facilities.
The private sector showed lower availabilities at 45 per cent of Tanzanian, 82 per cent of Uganda, 72 per cent of Kenya and 15 per cent of Zambian facilities.
Ultrasound scans had availability levels below 50 per cent in all sectors (public and private hospitals) of all countries, except the mission sector of Uganda (57 per cent).
Foetal scopes were commonly available in the public sector of Tanzania (97 per cent), Uganda (96 per cent) and Zambia (80 per cent), but not in Kenya (35 per cent).
Availability in the private and mission sectors showed a more mixed picture, with availabilities ranging from 16 per cent (private, Zambia) to 96 per cent (mission, Uganda).
Safe delivery kits were not at all available in Kenya and Uganda, and only 16 per cent of Zambian facilities. Tanzania had a much more elaborate availability at 82 per cent of public, 32 per cent of private and 33 per cent of mission facilities.
The availability of antiseptic was similar in Tanzania (65 per cent), Uganda (61 per cent) and Zambia (63 per cent), but lower in Kenya (24 per cent).
Vasectomy and tubal ligation kits were mostly unavailable in the four countries, with all overall availabilities below 10 per cent
Mr Kibira said most of the sexual reproductive health commodities were unavailable in most facilities because the governments were not budgeting enough for them.
“These are essentials that each country should have in place but most countries are not considering them as a priority hence the stock-outs,” he said
In the recommendation, Kenya was asked to adopt a multi-sectoral approach in the
provision of health services and commodities, especially in the rural and hard to reach areas, by integrating and bringing services closer to the population.
“County governments should include all the drugs as essential medicines by making budget available for their purchase,” recommends the study.
For Uganda, the government has been asked to actively seek out strategies to reduce the cost of high-cost SRHC such as magnesium sulphate, for instance through offering subsidies.
“Strategies to improve the SRHC supply chain must be actively sought to ensure that commodities are delivered on time and in the quantities ordered. Healthcare providers to receive additional training on SRHCs, especially in the private and mission sector facilities,” states the study.
The Zambian government has been urged to increase the number of trained staff, and improve the knowledge of existing staff and also improve the supply chain of the commodities.
For Tanzania, inadequate availability of SRH commodities, frequent stock-outs, poor logistic management, and limited community knowledge constituted major factors contributing to the problems experienced with accessing SRH commodities in the country
The government was, therefore, asked to ensure all the commodities on the international Essential Medicines Lists (EMLs) are also included in the Tanzania EML and sensitise communities about SRH services and commodities.








